Winter, 2000: The long nights of studying, and the culture shock of medicine, had left me feeling exhausted and uncertain as I completed first year of medical school. Had I made the right decision? How am I possibly going to learn everything that I need to know to become a doctor? Fortunately, I had scheduled a mindfulness retreat at Plum Village meditation center in France with Zen Master Thich Nhat Hanh that summer. I met with Sister Dang Nghiem, a former physician-turned-Zen-nun, and author of Mindfulness as Medicine, who has become a teacher and inspiration for me. I asked her, “How can I find time to develop my mindfulness and meditation practice when I have so much medical studying to do? I feel like every piece of medical knowledge I learn could save someone’s life someday, and there aren’t enough hours in the day to study, much less to practice meditation.”
She breathed calmly, paused, and turned to me. She said, “Think about the lives that you might be able to save if you can learn to be truly present for every person you are caring for.” That moment was a wake up call for me, and I decided then and there to do my best to bring mindfulness into the heart of my life as a human being, and my work as a healer.
What is Mindfulness?
The Pali word sati, that is translated into English as “mindfulness” has a history thousands of years old, going back to Buddhist meditation and other Eastern contemplative practices. That said, you certainly don’t need to be a Buddhist to practice and benefit from mindfulness. Communities throughout the world have long had something like mindfulness, even if they don’t use that word. Dr. Jon Kabat-Zinn at the University of Massachusetts defined mindfulness as “Paying attention in a particular way: on purpose, in the present moment, and without judgment.” “Mindfulness” is also sometimes translated as “heartfulness,” which highlights the inherent mindful quality of compassion. Decades of research have shown mindfulness to be a powerful tool for helping people cope with a variety of stress and illness, including chronic pain, anxiety, depression, and cancer.
Mindfulness is about staying present with whatever is happening in the present moment. It means not turning away from pain and suffering. I sometimes describe mindfulness as “Paying attention in a particular way: On purpose, in the present moment, and with unconditional love.” In this spirit, I cultivate my capacity to stay present with every situation, with compassion, both in pleasant situations as well as more challenging ones. Cultivating mindfulness can involve “formal” practices like sitting meditation or walking meditation, where we stop whatever else we are doing and focus on mindful awareness of our breath or our bodies. That same mindful presence can be practiced informally, at any time or place, including daily activities in the health care setting such as walking down the hospital corridor. Sometimes, before entering a patient’s room, I stop, take three slow mindful breaths, and remind myself, “This person is suffering. This is a sacred space that I am about to enter.” I do my best to let go of whatever may have just happened, and all of the things I still have ahead of me in the day. This simple practice helps me to stay present as I begin the next clinical encounter.
Calligraphy: Ly Hoang
Why Mindfulness for Health Care Providers?
One common stereotype of a mindfulness practitioner is someone who spends their time naval-gazing, self-absorbed, oblivious to the world. That image could not be further from my own experience of mindfulness as an active practice that helps me to engage in my clinical work with more focus and attention, and less distraction. Dr. Michael Krasner and Dr. Ronald Epstein at the University of Rochester have developed and researched mindfulness programs specifically for physicians. In a landmark study published in the Journal of the American Medical Association in 2009, they demonstrated that physicians who undertook a tailored 8-week intensive mindfulness training program showed less burnout, better mood and emotional stability, and improved physician empathy. Dr. Epstein and Dr. Krasner propose that mindful practice in medicine can impact three inter-related areas of care: (1) Quality of care (safe, timely accessible, effective, patient-centered); (2) Quality of Caring (empathy, compassion, responsiveness); and (3) Clinician well-being (improved mood, lower burnout).
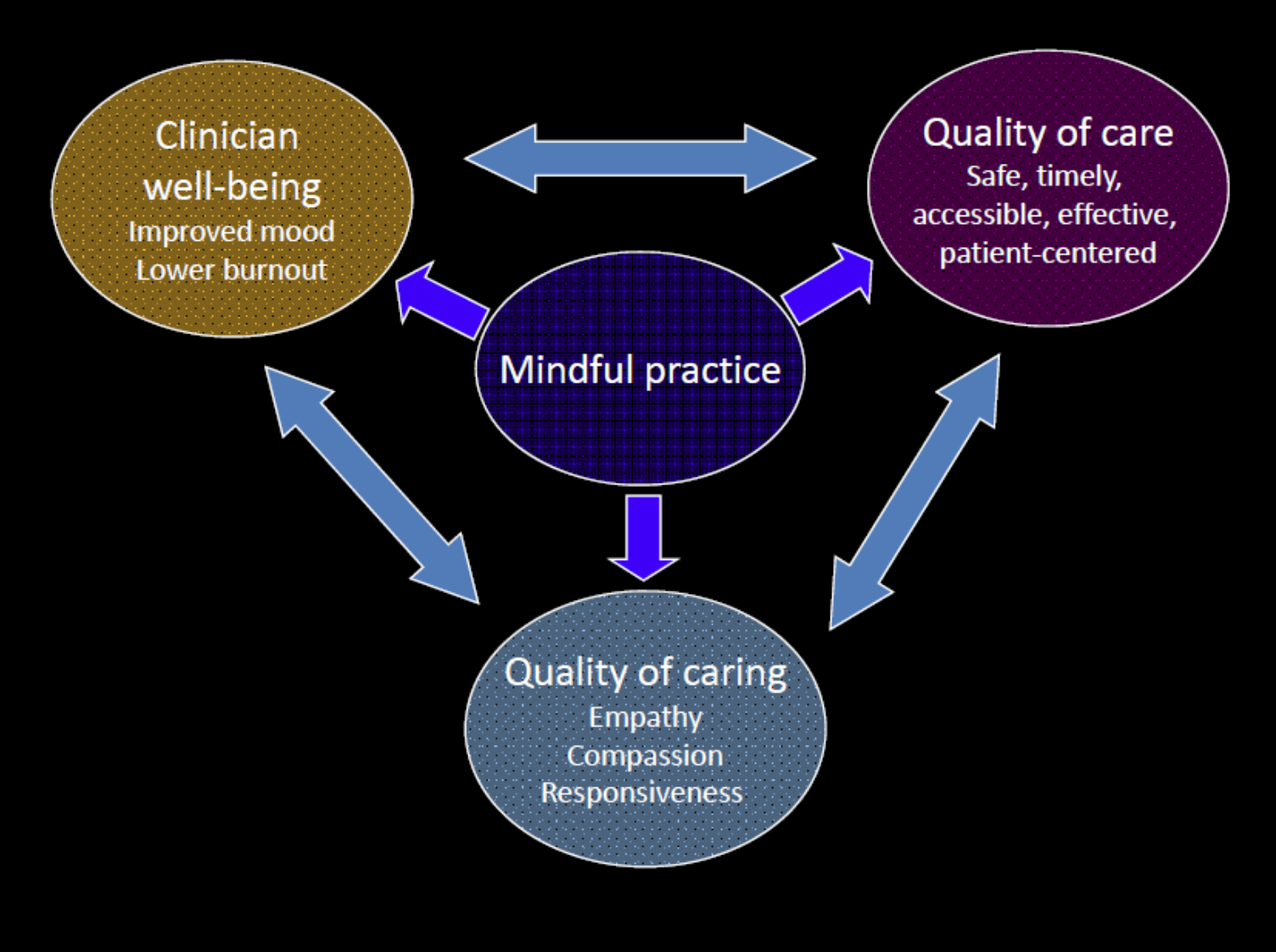
Reproduced with permission from Epstein RM & Krasner MS, Mindful Practice Facilitator Manual, 2017 https://www.urmc.rochester.edu/family-medicine/mindful-practice.aspx
&Krasner MS, Mindful Practice Facilitator Manual, 2017
Mindfulness practice improves the quality of care. When I was in medical school and learning how to conduct emergency “Code Blue” situations, a wise teacher told me to “Check your own pulse first” – even before checking the patient’s pulse! This lesson has stuck with me throughout my medical training and practice. I’ve found that when I am calm, centered, and fully present, I’m able to see what is really happening, think more flexibility, consider a wider range of possibilities, and make better decisions. On the other hand, when I am feeling rushed or inattentive or highly stressed, I’m more likely to miss important clinical information or make mistakes. When I’m mindfully aware of my stressed-out mental and physical state during my work day, that awareness gives me an opportunity to take a few moments to breathe, walk, and center myself, so I can better attend to the next patient or situation in front of me.
Mindful practice improves the quality of caring: Sometimes lost in our high-tech, intervention-focused health care system is the ancient healer’s art of compassionate communication and presence with patients. Master clinicians know, however, that earning trust and effectively caring for patients who are suffering requires a high level of compassion – the capacity to face, stay present with, and relieve, suffering. A trusting and compassionate clinical relationship is necessary for optimal communication and care. Moreover, the “bedside manner” of the clinician has an enormous impact on how patients experience illness and healing.
One of the most powerful (and challenging!) of mindfulness practices is mindful communication. When I’m listening mindfully to a young person or family, instead of interrupting or forcing through my own agenda, my primary intention is to be present with them. I want to really hear what they are saying, to attend to what they are experiencing emotionally, and allow them to feel fully heard and understood. When I am speaking mindfully, I bring a heightened awareness to what I am saying and how I am saying it, in the moment, with the primary intention of generating compassion and relieving suffering.
Sister Dang Nghiem wrote, “If a doctor learns to practice mindfulness … and she walks in quietly, peacefully, that’s already medicine. She’s calm. She’s not outside of her body. The patient feels that attention, that tenderness, that care, that true presence. The patient is already soothed.” I’ve also found that the practice of mindful communication has helped me to manage some extremely difficult situations with youth and families in crisis, and to defuse and de-escalate conflicts in the health care setting.
Mindful practice improves clinician well-being. Studies have shown that almost 50% of physicians experience significant symptoms of burnout at some point in their careers, and are at significantly increased risk for suicide and substance abuse compared to their peers. All health care professionals in every field and discipline face similar challenges. This is hardly a surprise given the pace and pressures of the modern health care environment. Adding to this, we are confronted with pain and suffering among people we serve, on a daily basis, and to a degree that is hard to imagine for most our non-medical family and friends. These experiences put us at high risk for “secondary trauma.” If we do not know how to handle these experiences wisely, we risk “absorbing” our patient’s trauma both physically and psychologically, which degrades our physical and mental health, and impairs our ability to be at our best in our clinical work and in our lives.
For me, mindfulness practice is a powerful tool for me to take care of myself, and to increase my own resilience. When I practice mindful walking on the way to work, I can let go of my anxious “to-do” list for the day, and arrive more refreshed and alert. When I practice sitting meditation after the death of one of my patients, I hold my heart in my hands, breathe with self-compassion, and allow myself to experience, and let go, of whatever emotions are arising in me in that moment. This allows me to continue serving as effectively as I am able to.
As clinicians and healers, our clear and compassionate presence is one of the greatest gifts that we can offer to our patients – just as much as our scientific knowledge and our technical skills. We have the opportunity to tap into, and strengthen, this capacity through the practice of mindfulness. Mindful providers will heal the world.
Resources
For me, developing my mindfulness practice has become a lifelong path full of joy and reward. Those new to mindfulness might enjoy Dr. Jon Kabat-Zinn’s Mindfulness for Beginners, or Thich Nhat Hanh’s The Miracle of Mindfulness. Dr. Ronald Epstein’s Attending: Medicine, Mindfulness, and Humanity is a masterpiece that makes the case for bringing mindfulness into the practice of health care. That said, reading about mindfulness is no substitute for experiencing it yourself, with the guidance of a skilled and experienced teacher. The BC Children’s Hospital Centre for Mindfulness is developing and offering mindfulness programs for health care professionals. Please contact mindfulness@cw.bc.ca for more information.